Non-restorative cavity control
Non-restorative cavity control
Suitable for:
- a primary tooth with arrested caries or when the tooth is unrestorable or close to exfoliation, and with no signs or symptoms of infection
- a primary tooth with an advanced lesion with no signs or symptoms of infection, where alternative methods are not feasible
Aim: To reduce the cariogenic potential of the lesion by altering the environment of the plaque biofilm overlying the carious lesion through brushing and dietary advice.
For lesions that are not readily cleansable (e.g. where dentine is not exposed or there are enamel overhangs) the lesion shape should be altered. Making the lesion cleansable may aid plaque control but there is no evidence of the effectiveness of this approach. Children might find this more acceptable than more invasive techniques, although success is wholly dependent on the child and parent/carer changing oral health behaviours (see Behaviour change). Therefore, the decision to use this management technique must be made on an individual patient basis, assessing the risks and potential implications of caries progression.
Show the parent/carer and child the carious lesions and explain the proposed treatment and the important role that they have in its success. Confirm that the parent/carer is in agreement with this approach.
Ensure that the child or young person, or in the case of younger children their parent/carer, are made fully aware of their role and responsibility for the success of this approach.
If necessary, make the lesion cleansable (refer to technique below).
If this approach is acceptable and agreed, provide site-specific prevention as follows.
- Demonstrate effective brushing of the lesion (e.g. to brush a multi-surface lesion may require the brush to be moved laterally).
- Give dietary advice.
- Apply fluoride varnish to the lesion four times per year.
- Consider the application of silver diamine fluoride.
Keep a record of the site and extent of the lesion to enable active surveillance and an alteration of the treatment plan if the lesion does not arrest, for example, via radiographs or photography (see SDCEP Oral Health Assessment and Review guidance for further details).
Record details of the agreed treatment in the patient’s notes. At each visit, assess for the presence or absence of plaque biofilm on the surface of the lesion and consider recording plaque scores (see Assessing toothbrushing). If the child, or parent/carer cannot keep the lesion free from plaque, consider an alternative management strategy.
Review the lesion after three months and if active lesions are not arrested (or showing signs of arresting) or previously inactive lesions have become active, consider an alternative strategy.
- For non-restorable teeth, this will be an extraction.
- For restorable teeth, see Management of caries in primary teeth flowchart.
Continue to provide Enhanced Prevention as described in Caries prevention.
Technique for making a lesion cleansable
As only enamel and carious dentine are removed, the use of a local anaesthetic should not be necessary unless subgingival tooth preparation is required.
Using a high-speed handpiece, or hand instruments, remove undermined enamel adjacent to the carious lesion making the surface of the lesion accessible to toothbrushing.
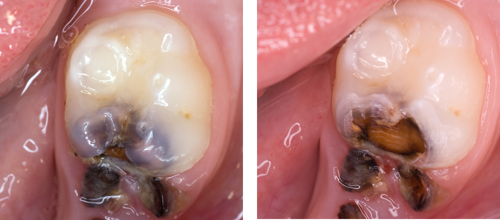
Images show a tooth before (left) and after (right) removal of adjacent undermined enamel to make a carious lesion cleansable.
The resulting cavity form will vary in shape depending on the lesion. Extreme care is required to avoid iatrogenic damage to the mesial of the first permanent molar when rotary instruments are used (see Avoiding iatrogenic damage).

Image shows a carious lower E managed with a prevention alone strategy. This has not been successful as plaque is visible four months later and the caries appears active rather than dark, hard and inactive (arrested). Therefore, a more restorative based approach is now required.